Professor Guilherme Del Fiol
Textbook: No textbook. Extensive readings were from the primary literature and Internet resources.
For me this was definitely one of the two or three most
important courses in the program. Lack of integration and interoperability is one of the two great barriers that prevent health information technology from reaching its full potential and providing all its expected benefits. I see this every day in my professional life. I can view data in my hospital’s electronic medical record using a portal system, but the only way to actually transfer that data into my office EMR is to print it out onto paper and scan it back into the target system where it becomes an inert, non-searchable image file. It is not unusual for my colleagues and I to order wasteful duplicative laboratory and radiologic testing because we have no way to know that the test we need was recently done or to obtain the result.
Current generation EMR’s lag far behind systems used in other fields such as industrial, financial, and even personal computing. To a very
significant extent, this represents apathy or even opposition by major EMR vendors to developing and promoting the shared terminology and data structures that would enable interoperability. The technical challenges are not insurmountable, but the vendors continue to claim that health information technology is somehow qualitatively different from commercial and consumer products in order to protect their prices and market share and prevent innovators from entering the market. The Office of the National Coordinator for Health Information Technology has dispensed hundreds of millions of dollars in grants to support a Nationwide Health Information Network backbone and the development of state and local Health Information Exchanges, but this technology will not be really useful until healthcare processes and data are liberated from
the narrow single-institution EMR environments where they are now forced to reside. An excellent paper in the June 14, 2012 New
England Journal of Medicine titled "Escaping the EHR Trap -- The Future of Health IT" by Kenneth Mandl and Isaac Kohane which discusses these issues in more depth is available at Escaping the EHR Trap — The Future of Health IT — NEJM.
significant extent, this represents apathy or even opposition by major EMR vendors to developing and promoting the shared terminology and data structures that would enable interoperability. The technical challenges are not insurmountable, but the vendors continue to claim that health information technology is somehow qualitatively different from commercial and consumer products in order to protect their prices and market share and prevent innovators from entering the market. The Office of the National Coordinator for Health Information Technology has dispensed hundreds of millions of dollars in grants to support a Nationwide Health Information Network backbone and the development of state and local Health Information Exchanges, but this technology will not be really useful until healthcare processes and data are liberated from
the narrow single-institution EMR environments where they are now forced to reside. An excellent paper in the June 14, 2012 New
England Journal of Medicine titled "Escaping the EHR Trap -- The Future of Health IT" by Kenneth Mandl and Isaac Kohane which discusses these issues in more depth is available at Escaping the EHR Trap — The Future of Health IT — NEJM.
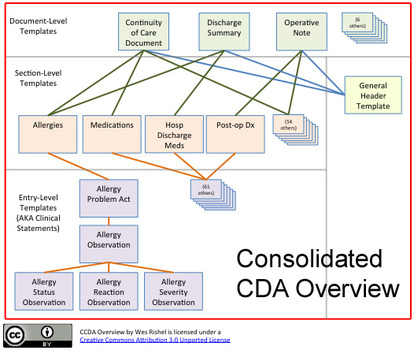
The class readings and discussion boards gave us a wide-ranging perspective on the concepts and technologies currently being used to facilitate communication between EMR systems. We studied the characteristics of healthcare data sets, information architecture, and the meaning and importance of syntactic and semantic interoperability. We also studied controlled standard terminologies, such as ICD 9-10, CPT 4, LOINC, SNOMED-CT, UMLS, and RxNORM, and did coding exercises in several of them. Finally we studied data and messaging standards including a
detailed examination of the difference between HL7 v 2.x and v 3.x, the nature of the v3.x Reference Information Model, the structure and contents of the Continuity of Care Document, and the next generation Consolidated Clinical Document Architecture. We also looked briefly at clinical decision support standards such as HL7 and the Arden Syntax.
detailed examination of the difference between HL7 v 2.x and v 3.x, the nature of the v3.x Reference Information Model, the structure and contents of the Continuity of Care Document, and the next generation Consolidated Clinical Document Architecture. We also looked briefly at clinical decision support standards such as HL7 and the Arden Syntax.
My project group, including Amy Andrade, Lisa Bedner, and Miriam Bucio-Vinkler, elected to study and write our major paper on the details of forming of a Regional Health Information Organization (RHIO) to allow the timely, accurate, bidirectional exchange of multiple types of clinical data among all stakeholders in a community (link attached). This required extensive research and many decisions on the terminologies and standards to be used, the information flow and architecture, the construction of an enterprise master patient index that achieves unique patient identifiers and accurate record matching, and the protocols to ensure the privacy and security of protected health information. We looked at the way existing RHIO’s were solving these problems and at whether there was sufficient high-quality data in the literature to define best practices in these areas. We tried to work at a granular level and provide details of how we would solve the problems if we were actually implementing the plan. I really enjoyed working on this project, and it generally supported my conclusion that while formidable problems remain, useful health information exchange is not as difficult as the EMR vendors assert.